An aneurysm is a weakened area in a blood vessel wall that can bulge and may rupture. If it ruptures in the brain, it causes bleeding, leading to a haemorrhagic stroke.
What is a stroke?
A stroke is a medical emergency and a life-threatening condition that occurs when part of the brain does not have adequate blood flow, most often due to a blocked artery or bleeding in the brain. Without a consistent blood supply, brain cells in the affected area begin to die from a lack of oxygen. The effects of a stroke can vary widely depending on the area of the brain affected and the severity of the interruption.
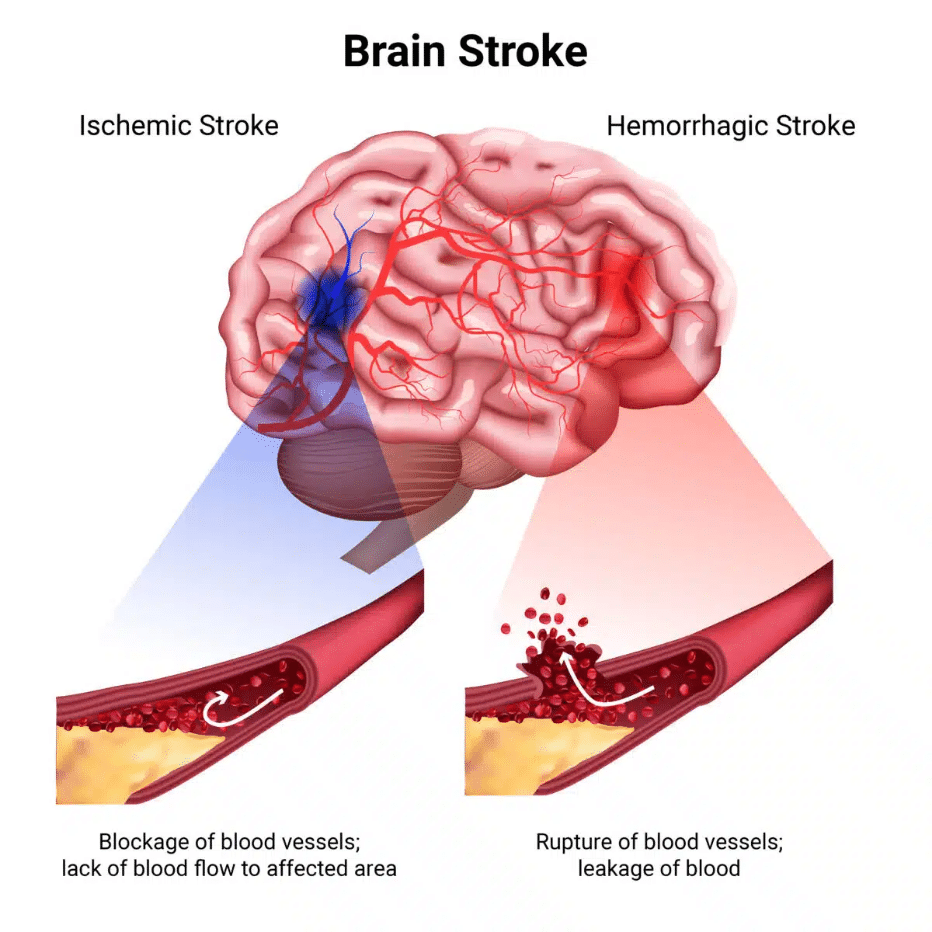
Strokes are often categorised as either:
ISCHEMIC STROKE
This is the most common type, accounting for approximately 87% of all cases. It occurs when one or more blood vessels in the brain become narrowed or blocked, leading to a significant reduction in blood flow.
HEMORRHAGIC STROKE (BRAIN HEMORRHAGE)
This happens when a blood vessel in the brain leaks or ruptures, leading to bleeding in or around the brain. It is often caused by weakened blood vessels, which can result from conditions such as an aneurysm (a bulge in the vessel wall) or an arteriovenous malformation (AVM), a network of abnormal blood vessels. High blood pressure adds extra stress on these fragile areas, significantly increasing the likelihood of a rupture.
TRANSIENT ISCHEMIC ATTACK (TIA)
Often referred to as a “ministroke”, TIA causes temporary stroke-like symptoms. Although brief, it is a warning sign of a possible future stroke. A TIA is considered a medical emergency, and a person should seek medical care as soon as possible.
RECURRENT OR SECONDARY STROKE
A secondary stroke, or recurrent stroke, occurs when a person who has already experienced a stroke suffers another one.
More than 80% of strokes are preventable yet each year, over 1.8 million people in Europe experience a stroke, with many at risk of a recurrent one. Taking action today can make all the difference in reducing your risks.
Key Definitions
An artery is a blood vessel that carries oxygen-rich blood from the heart to the rest of the body, including the brain. When an artery leading to or within the brain becomes blocked by plaque buildup or a blood clot, it can restrict or stop blood flow, increasing the risk of stroke.
The carotid arteries, located on each side of the neck, deliver oxygen-rich blood to the brain. In carotid artery disease, plaque builds up inside these arteries, reducing blood flow to the brain. Over time, the plaque can break open (rupture), triggering a blood clot. The blood clot can prevent blood flow through the carotid artery, or a fragment of the clot or plaque can break loose and travel to smaller brain arteries, causing a blockage there. Any of these scenarios can lead to an ischemic stroke, with carotid artery disease accounting for up to 30% of all such cases.
A blood clot is a clump of blood that forms to stop bleeding. However, if it blocks blood flow to the brain, it can lead to a stroke.
Plaque is a buildup of fatty deposits in the arteries that can narrow blood vessels and restrict blood flow. Plaques can also rupture, leading to blood clot formation.
ACT F.A.S.T.
Every second counts. Use the F.A.S.T. acronym to recognize the warning signs of a stroke and take action immediately:

Face drooping
Ask the person to smile. Does one side of the face droop or appear uneven?

Arm weakness
Ask them to raise both arms. Does one arm drift downward or seem weaker than the other?

Speech difficulty
Ask them to repeat a simple phrase. Is their speech slurred, garbled, or unusual?

Time to act
If you notice any of these signs, call the local emergency number immediately.
CAUSES AND RISK FACTORS
Understanding your risk is key to stroke prevention. There are two types of risk factors: modifiable (those you can manage, treat and improve) and non-modifiable – those beyond your control. The more risk factors you have, the higher your chance of having a stroke.

Reducing stroke risk in women
- Monitor blood pressure and manage pregnancy health.
- Be cautious with contraceptives and hormone therapies.
- Maintain a heart-healthy lifestyle: balanced diet, regular exercise, no smoking.
- Recognize stroke symptoms and seek help immediately.
Proactive steps and awareness can significantly reduce stroke risk and improve outcomes for women.
SIGNS AND SYMPTOMS
Recognizing the signs and symptoms of a stroke is crucial for seeking immediate medical help. A stroke often comes on suddenly, and the faster the intervention, the better the chances of recovery. Delaying medical care significantly increases the risk of permanent damage or even death.

HOW STROKE AFFECTS YOUR BODY AND MIND?
A stroke can have sudden, wide-ranging effects on both body and mind. Each person’s experience is unique — some may face mild, temporary effects, while others encounter more severe, lasting challenges. The type and intensity of these effects depend on which area of the brain is affected.
Here are the primary areas impacted by a stroke and the challenges that may arise:

Early Treatment and Management of Stroke
Emergency treatment is crucial for improving outcomes after a stroke, and the approach depends on whether the stroke is ischemic or haemorrhagic.
ISCHEMIC STROKE
The primary treatment goal of an ischemic stroke is to either dissolve or remove the clot to restore blood flow.

To break up the clot, doctors may administer an intravenous thrombolytic within 4.5 hours of symptom onset. These medications, sometimes referred to as “clot busters”, work by dissolving the clot, allowing blood to flow back to the affected area of the brain.
For larger clots, doctors may use a procedure called a mechanical thrombectomy. This involves threading a catheter through an artery in the groin to the blocked artery in the brain. A device, such as a wire-cage stent retriever, opens and grabs the clot, allowing it to be removed. This procedure can be done within 6 to 24 hours of symptom onset, depending on individual eligibility and may follow alteplase treatment if appropriate.
HAEMORRHAGIC STROKE
The primary goal of early treatment for a haemorrhagic stroke is to stop the bleeding, reduce pressure on the brain, and prevent further complications. Common treatment approaches include:
For some patients, minimally invasive procedures are an option. A small tube (catheter) with a camera may be threaded through a major artery in the arm or leg and guided to the site of the bleed in the brain. This allows the surgeon to see the affected area in detail and place a mechanism, such as a coil, to prevent further bleeding. These procedures are less invasive than traditional surgery and can help stabilize the condition.
In other cases, more extensive surgery may be required to repair the damaged blood vessel. For example, a surgeon may close off the base of an aneurysm to prevent additional bleeding.
High blood pressure is a common cause of haemorrhagic stroke. Medications are administered to lower blood pressure and reduce the risk of additional bleeding. The European Stroke Organisation (ESO) recommends starting antihypertensive treatment as early as possible, ideally within two hours of symptom onset, to safely lower blood pressure. The goal is to reduce systolic blood pressure to below 140 mm Hg while keeping it above 110 mm Hg to maintain adequate blood flow to the brain.
LIFE AFTER STROKE
Recovery is a journey of transformation, where you take control and redefine what this new chapter means for you. While every stroke impacts life differently, with the right support, rehabilitation, and lifestyle adjustments, many people rebuild their lives. The greatest progress often happens in the first few months, but recovery can continue for years, offering ongoing opportunities for improvement.
Rehabilitation is crucial for stroke recovery, aiming to help you regain independence and improve your quality of life by addressing physical, cognitive, and emotional challenges. Rehabilitation is not a one-time event — it starts as soon as it is needed and can continue for as long as you benefit from it, sometimes for years.
In Europe, there are several options for rehabilitation, depending on your needs:
- In-patient rehabilitation centers: Intensive therapy in specialized facilities, often within hospitals.
- Out-patient clinics: Regular therapy sessions while living at home.
- Home-based rehabilitation: Therapy provided in the comfort of your home.
What to expect in rehabilitation
At a rehabilitation center, your recovery is the priority:
- Personalized plans: Tailored therapy to meet your specific needs and goals.
- Dedicated team: Including doctors, physical therapists, nurses, occupational therapists, speech pathologists, dieticians, and other specialists.
- Specialized facilities: Equipped spaces for therapy and recovery activities.
- Skill building: Focus on relearning daily tasks, improving mobility, communication and cognition.
- Support and education: Guidance on recovery, stroke prevention and emotional well-being for you and your family.
Recovery from a stroke begins in the hospital with doctors and therapists and continues at home as you adapt to daily life and regain independence. This journey often requires embracing new routines and discovering practical ways to manage everyday tasks. Here are some important areas to prioritize as you move forward:
Home and independence
- Accommodation and home modifications: Adapt your home with handrails or ramps, rearrange furniture and rugs that could be obstacles to walkers or wheelchairs, and be sure doorways can open as wide as possible to make daily life easier and safer.
- Equipment for independent living: Tools like grabbers, shower chairs, and adapted cutlery can support independence and comfort.
Personal care and daily activities
- Bathing and personal care: Use bath seats, handheld showerheads, and long-handled sponges to make bathing easier. Consider simplifying grooming routines.
- Dressing: Choose loose-fitting clothing and use dressing aids, like button hooks or zipper pulls, to make getting dressed simpler.
Mobility and transportation
- Driving: Check with your healthcare provider about when it’s safe to drive again and whether you’ll need an assessment.
- Shopping: Use smaller, accessible stores or online shopping options. Bring someone to assist or use mobility aids as needed.
Healthy habits
- Physical activity and physiotherapy: Work with your healthcare provider and a physiotherapist to develop a safe exercise plan tailored to your abilities and recovery goals. This can help improve mobility, reduce pain, and support your overall rehabilitation journey.
- Healthy eating: Focus on a balanced diet with plenty of fruits, vegetables, whole grains, and lean protein to support recovery and prevent future strokes.
- Smoking: Quit smoking and reduce your exposure to second-hand smoke to lower your risk of future strokes and improve overall health.
Medication and risk management
- Managing medications: Keep a detailed list of medications, follow dosing schedules, and communicate with your healthcare team about side effects.
Work/ school, travel and relationships
- Returning to work or school: Collaborate with employers or educators to make necessary adjustments, such as flexible hours or assistive technology.
- Traveling: Plan carefully, including packing medications, informing airlines of your needs, and arranging accessible accommodations.
- Intimate relationships: Open communication with your partner is key. Take time to rebuild emotional and physical connections.
- Adapt your hobbies: Whether your interests are physical, creative or intellectual, find ways to modify your hobbies to suit your current abilities and focus on activities you love and bring joy to your recovery journey.
Parenting
- Balance recovery and parenting: Create a routine that allows you to focus on your recovery while meeting your children’s needs. Maintaining daily schedules will provide a sense of normalcy and security.
- Communicate with your kids: Be open with your children about your condition in an age-appropriate way, helping them understand what you’re going through.
- Involve your kids: Let children assist with simple tasks or therapy to feel included and empowered.
- Teach emergency skills: Show your kids how to recognize stroke symptoms and respond in an emergency. This preparation can alleviate anxiety about recurrent strokes.
- Adapt activities: Modify parenting tasks to suit your physical and cognitive abilities while staying actively engaged in your child’s life.
- Seek external support: Use community resources, counselling or support groups to help your family adjust.
Career planning and financial stability
- Consider new paths: If returning to your previous job is challenging, explore new career opportunities or educational programs that align with your post-stroke abilities and interests.
- Seek financial guidance: Research disability benefits, health coverage, or grants to manage medical costs and secure financial stability during your recovery.
Peer Support
- Connect with others: Join stroke survivor groups, especially those tailored to your age, to share experiences, exchange advice, and build a supportive community.
- Rebuild your social life: Stay connected with friends and family and consider adapting activities to suit your recovery needs while maintaining your social circles.
A stroke doesn’t just impact the body — it can also affect mental health and emotional well-being. It’s common to face challenges such as depression, anxiety, mood swings, and shifts in personality. Addressing emotional and behavioural changes is a vital component of stroke recovery. By proactively managing mental health, you can improve your quality of life and support your journey toward comprehensive rehabilitation.
Common emotional and behavioural changes after stroke:
- Depression: Persistent feelings of sadness, hopelessness and a lack of interest in activities once enjoyed. This is a prevalent condition among stroke survivors and can hinder rehabilitation efforts.
- Anxiety: Experiencing excessive worry, restlessness or fear, which can interfere with daily activities and recovery progress.
- Personality and mood changes: Notable alterations in behaviour, such as increased irritability, impulsivity or apathy, which may affect relationships and social interactions.
- Pseudobulbar Affect (PBA): Characterized by sudden, uncontrollable episodes of laughing or crying that don’t match one’s actual feelings, leading to social discomfort.
- Self-esteem issues: Feelings of inadequacy or diminished self-worth due to physical limitations or changes in abilities post-stroke.
Strategies for managing emotional health:
- Seek professional support: Consult mental health professionals familiar with post-stroke care to address emotional and behavioural changes.
- Engage in therapy: Participate in counselling or peer support groups to share experiences and develop coping strategies.
- Medication: Under medical guidance, consider medications that can help manage depression, anxiety or PBA symptoms.
- Healthy lifestyle choices: Maintain a balanced diet, engage in regular physical activity, and ensure adequate sleep to support mental health.
- Mindfulness and relaxation techniques: Practice meditation, deep breathing exercises, or yoga to reduce stress and enhance emotional well-being.
- Educate yourself and loved ones: Understanding the emotional effects of stroke can foster empathy and effective communication within your support network.
If you are caring for someone who has had a stroke, you might be wondering what the future holds. Recovery is a unique journey, with each person progressing at their own pace. Caring for someone after a stroke is both a responsibility and an opportunity to help them rebuild their life. Here are some tips to help you navigate this journey:
- Be there for them: Offer emotional support and be patient. Recovery takes time, and just being present can make a world of difference.
- Provide practical help: If you are unsure how to assist, ask them what they need most—whether it is help with daily tasks, attending appointments or simply spending time together.
- Encourage age-appropriate rehabilitation: Help them stay committed to therapy — whether physical, speech or cognitive — to regain abilities and boost confidence in their recovery.
- Encourage independence: While it’s important to help, let them do as much as they can on their own. This fosters confidence and aids in recovery.
- Stay connected with professionals: Keep in touch with doctors, therapists and social workers to stay updated on their progress and care plan.
- Monitor health: Keep track of their medications, watch for side effects, and report any new symptoms or concerns to their doctor.
- Address concerns about recurrent strokes: Create a family medical chart with emergency contacts and medical details to ease “what if” anxieties.
- Create a safe environment: Make adjustments at home to prevent falls, such as removing hazards, installing grab bars and improving lighting.
- Stay organized: Use a calendar to manage appointments, therapy sessions, and daily routines, making caregiving more manageable.
- Celebrate progress: Acknowledge small victories, no matter how minor they may seem. Celebrating milestones helps keep them motivated and optimistic.
- Facilitate social reconnection: Encourage them to rebuild social networks by participating in hobbies, community groups or online spaces for stroke survivors with shared experiences.
- Help plan for the future: Work together on their goals (such as career adjustments, education plans or personal aspirations), recognizing that their journey will be unique.
- Educate yourself: Learn about stroke recovery and the challenges they may face, so you can better understand and support their needs.
- Take care of yourself: Do not forget your own well-being. Make time to rest, eat well, and recharge. Caregiver support groups can provide valuable emotional support and advice.







































